Patellofemoral pain (PFP) represents about 25-40% of all knee injuries. It presents as anterior knee pain that is worse with stairs, squatting, jumping, running and after long periods of sitting. It is an injury that is often poorly rehabilitated and it is not uncommon for symptoms to persist for years after the initial onset.
Unfortunately, persistent symptoms often result in reduced levels of activity and in some cases physical activity is stopped all together, which has long term consequences for our general health.
The key to managing PFP pain is to address it early (anterior knee pain is common in adolescents) and rehabilitate it thoroughly. Most rehabilitation programs fail because they are not specific enough and are not continued for long enough to build the strength and endurance necessary for the knee to cope with the loading demands of everyday life.
So what causes PFP?
There is ongoing debate as to the cause of PFP, but a widely recognised theory is that mal-alignment or mal-tracking of the knee-cap (patella) alters the stress on the tissues of the joint between the patella and the femur.
Symptoms most commonly start with an overload situation. Too much, too fast, too hard is a common story in PFP.
Some of the risk factors for PFP are:
- Weak quadriceps muscles especially when there is an imbalance between the medial and lateral quadriceps muscles
- Weak gluteal muscles which effects the alignment of the thigh bone under the patella
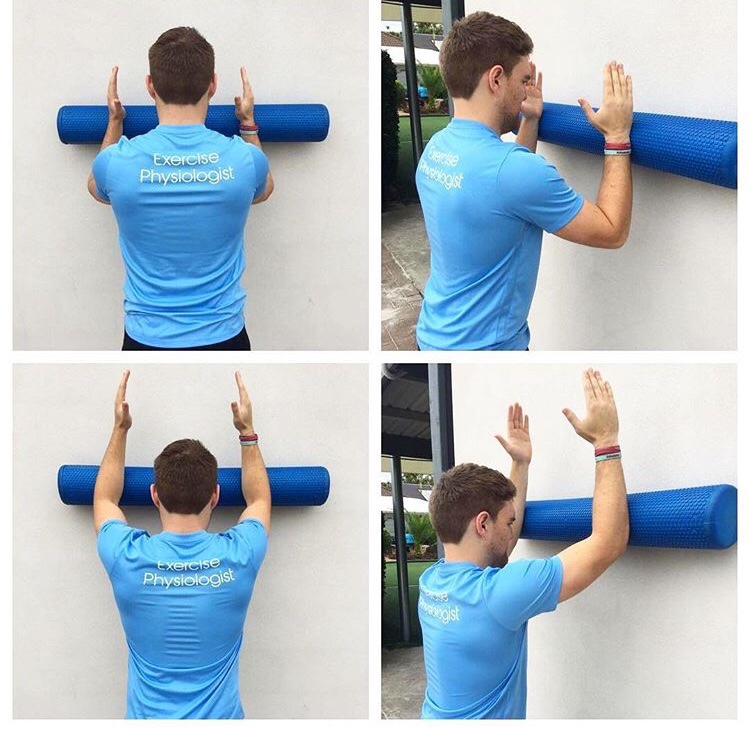
- Weak core and trunk muscles
- Weak calf muscles
- Foot pronation and poor dynamic function of the foot
- Tight hamstrings and calves
Pain is a big factor in perpetuating the patterns of weakness seen in PFP. Once the knee is symptomatic, the body alters its movement patterns and reduces the loading demands on the knee to avoid and reduce pain. This results in further de-conditioning of the relevant muscles and perpetuates a vicious cycle of chronic pain and weakness.
An accurate diagnosis is important as there are many causes of anterior knee pain and the rehabilitation of these other injuries differ slightly from PFP rehabilitation. Taping of the patella during the initial phases of rehabilitation is important to manage pain and allow the rehabilitation program to progress. Exercises that target all the relevant muscles in the lower limb and pelvic area need to be progressed as the symptoms improve and need to be continued until the strength of these muscles match the demands of your lifestyle.
Once again, rehabilitation of PFP often fails because the program is not specific enough and it is often stopped before the necessary strength gains are achieved.
A good physiotherapy rehab program for PFP should:
- Educate you as to what factors are contributing to your problem
- Advise you about appropriate activity modification during rehabilitation
- Set realistic expectations for how long the rehabilitation process will take - regaining the necessary strength in the appropriate muscles takes time!
- Motivate you to stay on board with the rehabilitation
- Manage your pain with hands on treatment and strapping
- Use foot orthotics where appropriate
- Address any biomechanics issues or technique issues in sport that are contributing to the problem
- Especially in Adolescents - manage pain early and rehab well! Remember studies have shown that symptoms can persist for years after initial onset and can predispose the joint to arthritic change in later years
In summary, a good physiotherapy program will:
- Unload
- Settle
- Improve movement patterns
- Reload.
This process takes time and patience and often requires an element of continued self-management to prevent re-occurrence of the symptoms.