Stress fractures commonly occur in sports where the movement demands of the sport produce repetitive loads on the body. Sports involving running, jumping and dancing place the individual at a higher risk of a bone stress injury. The incidence of stress fractures in the femur can range from 2.8% to 33% of all stress related injuries (both to the shaft and neck of femur). Management of these injuries requires an accurate diagnosis, often long periods of activity modification and rehabilitation (generally <4 months). The rehab program requires the close monitoring of a gradual and structured increase in load to allow the individual to return to full activity.
Stress fractures to the femoral neck are quite rare and are seen most commonly in long distance or marathon runners. While only accounting for a small percentage of all stress fractures they are considered to be quite serious given the length of time required for recovery and tendency to require surgical fixation if not addressed early. Differential diagnosis should therefore also consider other possible causes such as:
- Bursitis
- Tendonitis
- Muscle strain or injury
- Avascular necrosis
- Slipped capital femoral epiphysis
- Sacroiliac injury
- Acetabular and pelvic fractures
- Hip joint arthritis
- Perthes disease
- Femoroacetabular impingement (FAI)
What is a stress fracture?
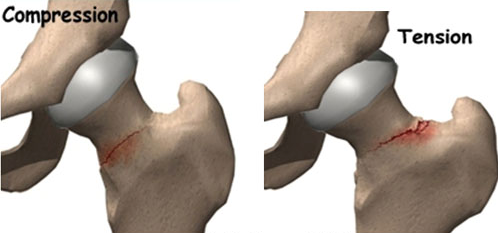
A stress fracture can occur as the result of fatigue failure of bone where the amount of microscopic damage from repetitive load exceeds the bones ability to repair and remodel. The femoral neck is particularly vulnerable due to the fact that the majority of vertical compression forces load through the femoral head, falling medially to the shaft of the femur. This creates a compressive load medially and tension load laterally.
A stress reaction, or fracture, occurs when there is a failure of the bone to remodel adequately with the addition of repetitive sub-threshold stress. This ability of bone to adapt to pressure, or lack of it, is known as Wolff’s Law and refers to the bones anisotrophic ability to manage load along multiple axes. Cortical bone, of which the majority of the skeletal system is comprised, is heavy and has a slow metabolic turnover which can increased the likelihood of stress related injuries. Especially when there is inadequate recovery time after exercise and loading.
Mechanical load on the bone in the form of intrinsic loading (stress) or mechanical deformation (strain) is required for bone remodelling to occur. When a stress injury occurs the bone is unable to cope with the excess amount of stress or strain.
Factors to consider when determining the effect a load may have on the skeletal system would include:
- Amount of load (volume, rate and frequency of load application)
- Bone health and geometry (bone mineral density and anatomical cross sectional area can be used as measures of this)
- Activity of surrounding muscle (where muscle strength and balance can have a protective effect on shearing loads)
Load on a bone can be classified as compressive, tensile or shear. When a bone bends it will experience a compressive load on one side and a tensile load on the contrary side. Usually a failure of bone integrity will occur on the tensile side. This can result in microscopic damage accumulating and fatigue failure of the bone occurring, described as “crack initiation” (Knaeding et al, 2005). Without adequate rest and recovery time, this process will continue towards a “crack propagation” which results in a macroscopic failure of the bone.
Causes
Risk factors for developing stress fractures can broadly be categorised as intrinsic or extrinsic in nature.
Intrinsic factors:
- Endocrine deficits (particularly in female athletes)
- Bone geometry and density
- Poor patterns of loading and pathomechanics
- Inadequate nutritional profile
- Vitamin D deficiency
- Overall physical fitness
Extrinsic factors:
- Recent changes to training variables (such as increased frequency, intensity and duration)
- Poor biomechanics
- Poor set up
- Poor or incorrect equipment use
- Footwear
- Environmental considerations
Diagnosis
Diagnosing a stress fractures of the femoral neck requires:
- A thorough history exploring known risk factors:
- Medications
- Diet
- Occupation
- If female, menstrual history
- Sudden increase in physical activity involving repetitive sub-maximal loads
- Pain in the region of the groin or proximal femur (and occasionally asymptomatic knee referred pain)
- Palpable pain of the hip joint and pain at the extreme end of range with passive hip joint movements
- An active straight leg raise and log roll test may elicit groin pain
- Functional tests such as single leg hopping have been shown to be positive in almost 70% of patients
- Imaging to confirm diagnosis:
- Plain x-rays, while often negative in the early stages may show periosteal callous formation and intraosseous sclerosis. Plain x-ray sensitivity has been shown to range from 12-56% (Wright et al, 2016)
- Gold standard is with MRI and/or bone scintigraphy. Sensitivity for bone scintigraphy is slightly less (50-97%) compared with MRI (68-99%) (Wright et al, 2016)
Table 1. Classification grade of stress fractures on MRI. *STIR – short tau inversion recovery
Femoral neck stress fractures can be classified as compression or tension type:
- Compression injuries generally occur at the inferomedial cortical bone of the femoral neck have better outcomes due to the reduced risk of displacement. These are usually managed conservatively with good outcomes
- Tension injuries generally occur at the superolateral aspect of the femoral neck have been shown to have poorer outcomes and display greater rates of displacement. Due to this increase risk they must be diagnosed early in order to prevent poorer outcomes. These can often progress to a displaced fracture and inevitably end up with surgical internal fixation
Delayed diagnosis has been shown to be associated with poorer outcomes in athletes. A study of 23 athletes with femoral neck stress fractures with follow up over 6 years following injury noted the most significant aspect of management was a delayed diagnosis with 13 athletes requiring internal fixation. The average time to confirming the diagnosis was 14 weeks after initial onset of symptoms. The injuries requiring fixation were career ending for all elite athletes in the study (Johansson et al, 1990).
Management and Rehabilitation
Successful conservative management of femoral neck stress fractures requires:
- early diagnosis
- a graduated return-to-sport protocol - guided by pain
The most important determinant to be made with femoral neck injuries is the site of stress. Lateral femoral neck injuries are considered a high-risk stress fracture compared with medial sided compression stress. As a result, a slower, more cautious conservative rehab approach should be taken with a longer recovery time for lateral sided compression injuries.
Management should be done in collaboration with a sports medicine physician who can address other possible intrinsic causes. Physiotherapy treatment is paramount as this will guide the athlete back to a sporting performance level. A guideline for time frames and loading is summarised in table 2.
Table 2. Time frames and guidelines for return to activity (Wang et al, 2015; Kaeding et al 2005)
Evidence for return to activity with femoral neck stress fractures is poor, lacking any substantial randomised control trials, and limited only to expert opinion based articles and case series (Wang et al, 2015). General consensus shows that a minimum period of 4-6 weeks of strict non-weight-bearing must be carried out until pain free. This can then be upgraded to partial weight-bearing, weight-bearing as tolerated and then followed by full weight-bearing.
Continual and regular assessment is important to ensure the pain does not return and that suitable loading and subsequent healing has occurred. Follow up radiographs can be done to ensure adequate healing without progression of a fracture line. Non-impact exercises can then be gradually introduced followed by low impact and finally running exercise is allowed. Progression through such loads is only allowed in the absence of pain. Regression of load is needed if pain returns.
If you are a runner and have noticed a gradual increase in hip pain with running training, contact us at The Physio Lab for an opinion and discussion on what the possible causes might be and further management options to prevent a potentially serious injury from occurring.
Kaeding, C.C., Yu, J.R., Wright, R., Amendola, A., Spindler, K.P. (2005). Management and return to play of stress fractures. Clinical Journal of Sports Medicine. 15(6), 442-7. doi: 10.1097/01.jsm.0000188207.62608.35
Wright, A.A., Hegedus, E.J., Lenchik, L., Kuhn, K.J., Santiago, L. and Smoliga, J.M. A (2016). Systematic Review with Evidence-Based Recommendations for Clinical Practice Diagnostic Accuracy of Various Imaging Modalities for Suspected Lower Extremity Stress Fractures. Am J Sports Med. 44(1), 255-263. doi: 10.1177/0363546515574066
Johansson, C., Ekenman, I., Tornkvist, H., & Eriksson, E. (1990). Stress fractures of the femoral neck in athletes: The consequence of a delay in diagnosis. Am J Sports Med, 18 (5), 524–528. doi:10.1177/036354659001800514
Wang, T., Matheson, G., and Safran, M.R. (2015) General Treatment Concepts for Stress Fractures. In Miller, T.L. and Kaeding, C.C. Stress Fractures in Athletes: Diagnosis and Management. Springer International Publishing, Switzerland doi: 978-3-319-09238-6